2 Anatomy of Skin
Learning Objectives
Test questions are written using concepts listed in the Learning Objectives.
- Describe the structure of the skin and the tissue types that comprise it. Distinguish between the epidermis, dermis, and hypodermis.
- Describe the characteristics of the stratum basale and stratum corneum in the epidermis. Compare and contrast the characteristics and functions of the keratinocytes in each layer.
- Describe the functions and locations of melanocytes, Langerhans cells, and Merkel cells.
- Describe the structure and function of the major cell types, fiber types, and skin appendages found in the dermis. Describe the location and function of the papillary and reticular layers of the dermis.
- Explain the significance of tension, or cleavage, lines of the skin (Langer’s lines).
- Describe the types of nerve fibers that are carried in cutaneous nerves. Define their targets.
- Describe what decubitis ulcers are and how they develop.
- Compare and contrast the layers of the skin that are involved in first, second and third degree burns as well as the basic clinical consequences of each type of burn.
- Describe the basic sequence of events in wound healing.
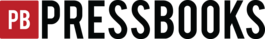
The skin is the organ of the body with which we are most familiar, and the one we most take for granted. It has many crucial functions. It forms a barrier to abrasion, infection, UV rays, and dehydration; it is a sensory organ and an excretory organ; it helps regulate body temperature and is necessary for the production of vitamin D. Structurally, skin has two layers: the epidermis, keratinized stratified squamous epithelium, and the dermis, a connective tissue network of collagen and elastic fibers containing blood vessels and nerve endings. The structure of the skin is highly specialized by region. In areas with increased friction, it is thicker and tightly fastened to underlying tissues. In areas where it is involved in grasping, the skin has prominent ridges (look at your fingertips!).
KNOWLEDGE CHECK
Structure of the Skin
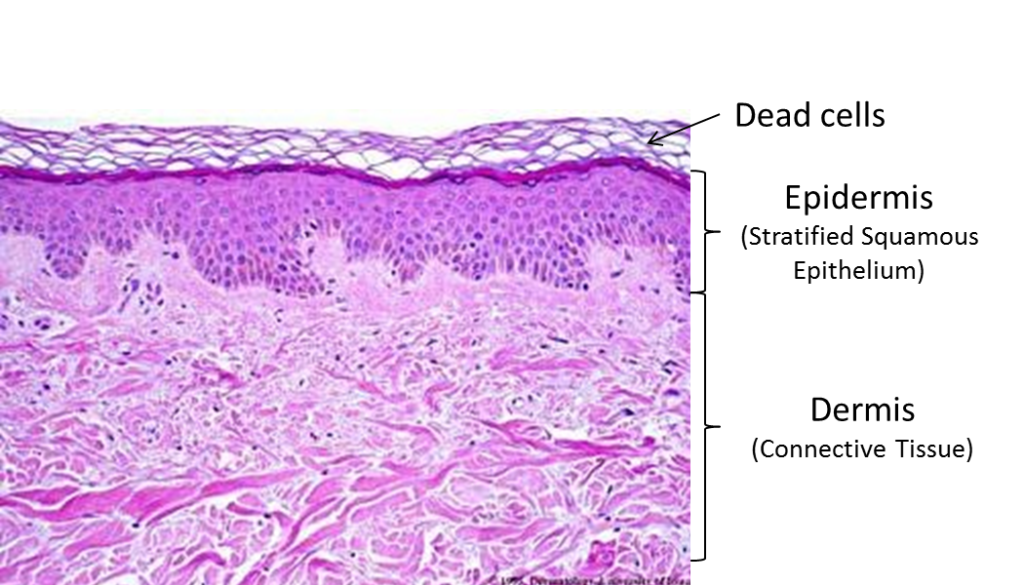
The skin is composed of two tissue layers, the outer epidermis and the inner dermis. The average thickness of the two layers is about 1/8 inch, but the actual thickness varies a great deal, based on the functional needs of different areas of skin. For example, the skin of the eyelids is about 1/16 inch thick, while the skin on the soles of the feet is more than 1/4 inch thick. You will appreciate these variations as you dissect different regions of the body.
The tissue layer deep to the dermis is called hypodermis. It is not considered to be part of the skin ‘proper.’ It is made primarily of adipose tissue and it varies greatly in thickness regionally (and between individuals).
KNOWLEDGE CHECK
Appendages of the Skin
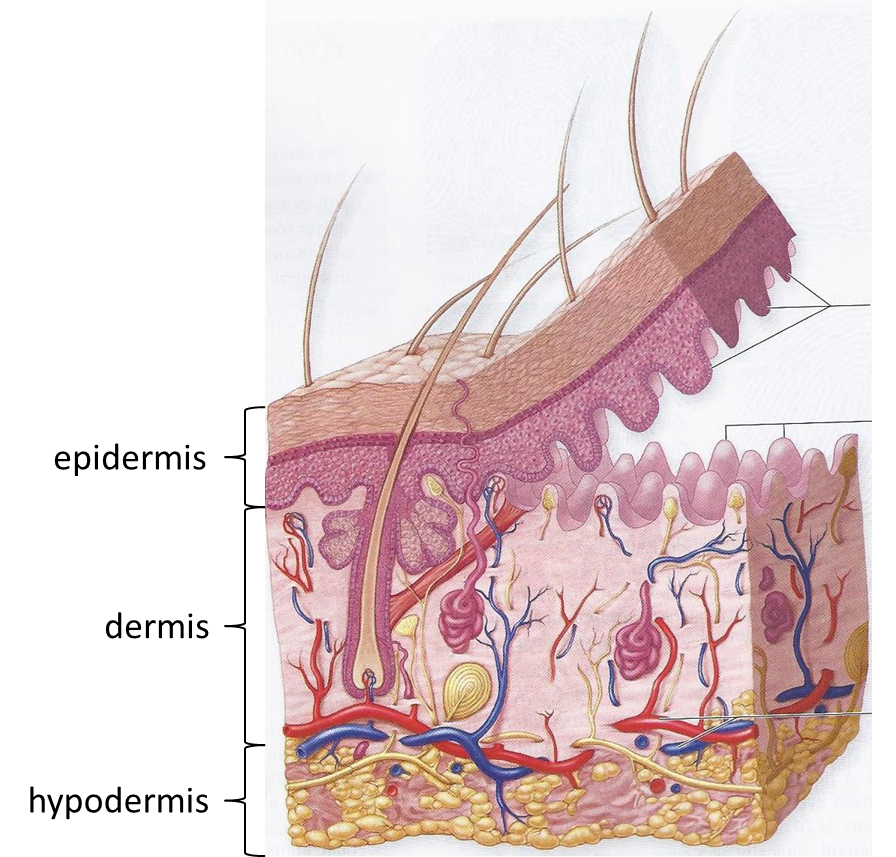
Nails, hairs, sebaceous glands and sweat glands are all derivatives of the epidermal layer of the skin. The nails are highly modified thickenings of the stratum corneum layer. Hairs and their associated follicles, sebaceous glands, and sweat glands are all derived from the stratum basale of the epidermis and are continuous with it, though all three types of structures grow into the underlying dermis (and may also extend into the hypodermis).
The continued growth of an individual’s hair is dependent on high mitotic activity of the stratum basale layer of the epidermis, from which the hair follicle is derived. High rates of mitotic activity are characteristic of many epithelial tissues. Many chemotherapy drugs that are used to treat cancer do so by destroying the most rapidly dividing cells in the body. Such drugs, in addition to interrupting the growth of cancer cells, destroy cells in the hair follicle, resulting in hair loss. After chemotherapy stops, the hair follicle can recover and hair will regrow.
Associated with each hair follicle, there is a very small smooth muscle, an arrector pili muscle. These muscles are innervated by the sympathetic nervous system. Contraction of the arrector pili muscles causes the individual hairs to stand on end (piloerection). This causes “goose bumps” in humans, which may occur when one is chilled or frightened. In animals, which have a thick covering of fur, the contraction of these muscles, and the erection of the hairs, creates a “dead air space” next to the skin that functions as a fantastic insulating mechanism. In other animals, erection of all the hairs makes the animal look larger and more ferocious, a defense mechanism.
The sympathetic nervous system innervates sweat glands and stimulates the production and discharge of sweat. It is worth repeating that individuals with spinal cord injuries cannot sweat at levels distal to the injury and they must use other strategies to take the place of the thermoregulatory function normally carried out by the sweat glands. (Dogs, pigs and some other mammals don’t sweat much because they do not have significant numbers of sweat glands. How do they cool off?)
KNOWLEDGE CHECK
Innervation of the Skin
As stated previously, innervation to the skin travels to and from the spinal cord via the spinal nerves and their branches, the dorsal and ventral rami. Innervation of the skin is segmental. Each spinal cord level receives sensory information from one strip of skin, a dermatome.
Nerves in the skin are cutaneous nerves and contain sensory and sympathetic fibers. Sensory fibers convey all sensation from the skin to the central nervous system (pain, touch, and temperature). Sympathetic fibers innervate sweat glands, arrector pili muscles, and the blood vessels of the dermis. Almost all innervation to the skin is in the dermis. With the exception of a few free nerve endings, the nerves do not reach the epidermis.
KNOWLEDGE CHECK
Burns
Burns are among the most traumatic of injuries. Besides causing tissue damage, burns breach the barrier functions of the skin, exposing the body to microorganisms and allowing significant fluid loss from the body, which can disrupt blood volume and organ function. Major burns cause homeostatic imbalances in every system of the body, a testament to the importance of skin function to the body.
One scheme for classifying burns is based on how many layers of tissue are injured:
- In first-degree burns, the epidermis is damaged, but not destroyed. First-degree burns are red and painful, but they are not serious. A mild sunburn is one example. There may be swelling, redness and pain. The injured cells peel off and the skin will heal, without scarring, in about two weeks.
- Second-degree burns destroy the epidermis and also cause some cell destruction in the dermis. Blisters appear and the surface is usually wet or moist due to plasma loss. There may be greater pain with second-degree burns than with third-degree burns (the most severe) because nerve endings in second-degree burns are still intact, but damaged. New skin can regenerate from the remaining dermis, but there may be scarring. If left untreated, a second-degree burn can lead to more severe tissue damage. All second-degree burns should receive medical attention.
- Third-degree burns destroy the epidermis and dermis, and can extend into the underlying hypodermis. Because nerve endings in the dermal layer of the skin are destroyed in third-degree burns, these burns may not be as painful as less severe burns. The burned area will be relatively dry, due to the loss of the blood vessels of the dermis, and often has a white or charred appearance. There is considerable loss of body fluids through these burns. Since the dermis is destroyed, the skin cannot regenerate. Surgery and skin grafts are always necessary.
KNOWLEDGE CHECK